People with sickle cell disease must cope with daily stresses and life-changing challenges. These stresses include family stress (children miss school, parents may lose their jobs), financial hardship, and pain episodes that can be life-threatening.
These events can also contribute to feelings of depression and a distrust of the healthcare system. Coping strategies are tools that help you deal with these situations.
Take Care of Yourself
Sickle cell disease can cause many physical and emotional challenges. Frequent pain episodes, hospitalizations, and absence from work or school can add to significant stress for families. Some patients experience depression, which can be treated with counseling and antidepressant medications.
People with sickle cell must also navigate stigmas associated with their condition and a lack of understanding from some healthcare professionals. Dana Jones, the mother of two girls with sickle cell, says she has witnessed healthcare workers in the emergency room accuse her daughters of faking their pain to get narcotic painkillers.
Patients and their families must have a robust support system to care for themselves. They must make sure they have regular checkups to help prevent serious medical complications.
During these appointments, patients and their families should practice healthy habits such as drinking plenty of fluids, eating well, getting enough sleep, and keeping up with vaccinations to help prevent infections. They should also be prepared for pain episodes by stocking up on nonsteroidal anti-inflammatory drugs (like ibuprofen) and taking acetaminophen, which can help control the acute pain. They should also learn how to palpate the spleen, which can be done daily or more often in a crisis, to see if it is more significant than usual, a sign of splenic sequestration.
Get Support
The pain that people with sickle cell disease experience and a higher risk of infection and complications in pregnancy and the cardiovascular system puts them at greater risk for depression and anxiety. Opening up about how sickle cell impacts mental health can spark a larger conversation and help drive change.
Support from family, friends, and sickle cell support groups can be crucial to a person’s quality of life. Precious attends sickle cell conferences nationwide to learn about the latest treatments, share her story, and connect with other patients and caregivers who know what she’s going through.
People with sickle cell often feel isolated, especially with pain crises. Others need to help, whether driving to the hospital or ensuring a friend has food and water when needed. It’s also essential for loved ones to learn how to palpate (feel) a child’s spleen since a splenic sequestration crisis can cause severe pain and be dangerous if left untreated.
Some medications can help prevent painful sickle cell crises. L-glutamine oral powder (Endari) helps to reduce these crises, and drugs like hydroxyurea (Droxia, Hydrea, Silkos), voxelotor (Oxbryta), and crizanlizumab-tmca (Adakveo) stop abnormal red blood cells from sticking together. Having enough fluids, sleeping well, and avoiding stress can lower the risk of sickle cell crisis.
Talk to Your Health Care Team
People with sickle cell often face stigma from others. This can lead to feelings of loneliness and hopelessness, worsening pain episodes.
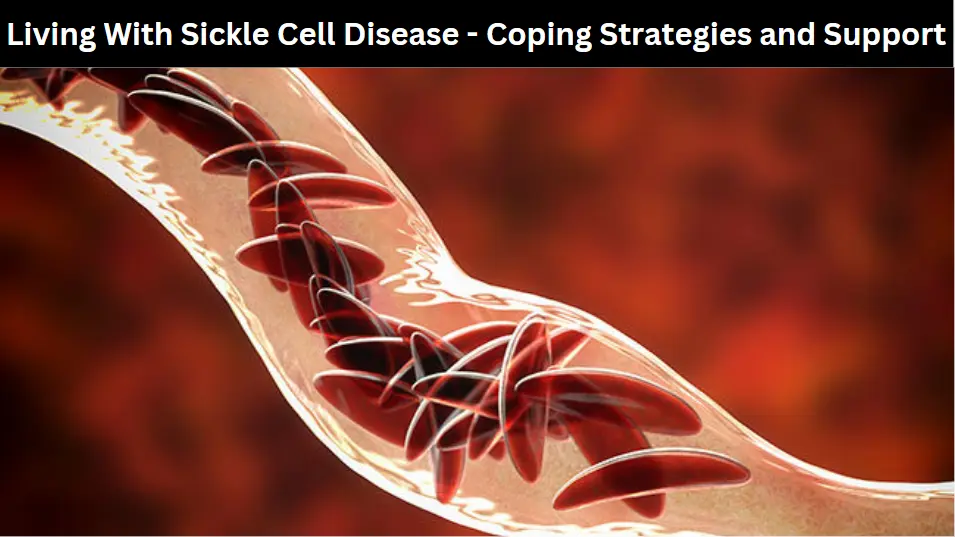
Sickle cell disease causes red blood cells to become rigid and sticky, like a sickle (C-shaped farm tool). When they move through the blood vessels, these hardened cells can block the flow, which causes pain and can cause problems in other organs, such as the heart and lungs.
Talking with your care team can help reduce these feelings and make coping easier. Your general practitioner (PCP), your extended healthcare team’s primary point of contact, can be an excellent place to start the conversation. Your PCP can also give you tips for managing your condition.
For example, your PCP may suggest you learn to palpate (feel) your spleen daily. This helps you identify when your spleen is at risk of becoming enlarged or having a crisis. Your PCP can also teach you how to use an app that enables you to record your pain and symptoms.
Your PCP can also provide information about various resources to help you live with sickle cell, including support groups and clinical trials for new treatments. Depending on your age and needs, you can also explore eligibility for Social Security disability benefits — sickle cell disease is one of the conditions listed.
Be Prepared for Painful Episodes
A sickle cell disease is a group of disorders caused by mutations in hemoglobin, the protein inside red blood cells. When hemoglobin takes a sickle or crescent shape, these abnormal cells get trapped in small blood vessels and block blood flow to essential organs, causing pain and other complications. It’s a chronic (long-term) condition, and people with it often need hospital care.
In addition to having frequent medical problems, people with sickle cell also deal with emotional stress. They may feel stigmatized because of how their blood disorder affects their appearance and health. They also often feel depressed because they have so many pain episodes, which can be scary and lead to hospitalizations. It’s important to talk about these feelings with your doctor. They can recommend resources to help.
It’s also essential to prepare for painful episodes by having a plan. Make sure family members, friends, and teachers know what to do if you or your child experiences a sickle cell crisis. Teach them to palpate your child’s spleen and call the doctor if it feels more significant than usual.
Ensure you and your child have a medicine bag with pain medicines, needles, fluids, a thermometer, and an emergency phone. Also, be prepared for crises by keeping a schedule of regular checkups with your doctor and making plans for getting help when you or your child gets sick.